- Clinical Observation of MEBO in Treating Skin Soft Tissue Injury of Distal Finger

-
目录
- 再生医疗技术治疗电烧伤的临床应用研究
- Clinical application of MEBT/MEBO in the treatment of electric burn
- 烧伤样本的临床特点及其表达
- MEBO在大面积烧伤晚期残余创面的临床应用
- MEBO包扎疗法治疗烧伤残余创面疗效观察
- 烧伤创面外用药物诱发局部过敏反应的临床处理
- 精神分裂症合并烧伤的临床护理
- 硫普罗宁对烧伤患者肝功能异常的治疗作用
- 湿润烧伤膏治疗手指末节皮肤软组织缺损的临床观察
- Clinical Observation of MEBO in Treating Skin Soft Tissue Injury of Distal Finger
- 人可调节封闭式负压引流技术治疗外伤创面的临床效果观察
- 美宝创疡贴治疗创伤性皮肤软组织缺损临床体会
- 美宝创疡贴治疗手术切口的疗效观察
- 湿润烧伤膏配合手术治疗合并组织缺损的手掌贯通伤
- 湿润烧伤膏配合加味骨碎补汤促进骨折愈合的临床研究
- 美宝创疡贴治疗骨折患者皮肤软组织挫擦伤
- 湿润烧伤膏在激光治疗静脉曲张术中和术后的临床应用
- 痔疮术后局部综合换药治疗的疗效分析
- 面部瘢痕的手术治疗
- 湿润烧伤膏联合美宝创疡贴在皮肤创疡治疗中的应用
- 美宝创疡贴联合湿润烧伤膏治疗慢性溃疡的临床观察
- 湿润烧伤膏联合远红外线治疗压疮的疗效观察
- MEBO外用联合口服芪黄通络汤治疗足踝部损伤性溃疡21例疗效观察
- 湿润烧伤膏治愈盲肠残端瘘1例报告
- 湿润烧伤膏治疗阑尾炎术后切口感染观察
- 湿性医疗技术与常规方法处置慢性肥厚性鼻炎激光术后创面效果比较
- MEBO处理宫颈环形电切术后创面的疗效观察
- 肝细胞移植解决α1抗胰蛋白酶缺乏
- Wild-type Hepatocytes transplantation for α1-Antitrypsin deficiency
HE Ren-liang, LI Feng-chun, CHENG Peng
Affilitions: Department of Skin Burns, Traumas and Ulcers, Huangpu People's Hospital of Zhongshan City, Zhongshan 528429, Guangdong Province, China【Abstract】 Objective To observe the effect of MEBO in repairing skin soft tissue defect of distal fingers. Methods A total of 174 fingers in 105 cases with distal finger skin soft tissue injury were treated with MEBO after simple wound debridement. Results All the 174 fingers of 105 cases were repaired with a favorable rate of 87.93%, and no case required skin grafting or flap repair. Conclusion MEBO has favorable effect on the skin soft tissue injury of distal fingers, especially on the defect of the V area.
【Key words】 MEBO; Distal finger; Skin soft tissue injury; TreatmentOf the emergency traumas, hand injuries account for a percentage of 15.0% to 28.6%[1,2], while of the emergency bone traumas, hand injuries account for 40%[3]. Moreover, soft tissue injuries of the fingertips occur more frequently, accompanied by soft tissue defect and bone exposure. Traditionally, the degloving injury of fingertips is treated by residual wound repairing or pedicled skin tube repairing, but the post-operative restoration of the outline and function is unfavorable[4]. From March 2005 to March 2010, we used MEBO to treat 174 fingers of 105 patients with fingertip soft tissue injuries and the clinical efficacy was very good. Unnecessary finger amputation was avoided and the lengths and functions of the fingers were remained. We report the cases as follows.
1. Clinical data
1.1. General data
We treated 174 fingers from 105 patients, including 72 males and 33 females of 4 to 61 years old. We found single finger injury in 127 cases, double fingers injuries in 19 cases and three fingers injuries in 3 cases (Injuries caused by extrusion of the whole hand). There were injuries with 31 thumbs, 64 index fingers, 52 middle fingers and a total of 27 ring fingers and little fingers. The injuries were mainly caused by cutting, punching and extrusion, chainsaw, stone pounding, etc.
1.2. Classification and grading criteria
In accordance to the classification criteria of distal finger defect by XIANG Li-yuan et al[5], there are five zones and three grades based on the wound surface and injury types, i.e. Zone I: from the distal 1/3 area of the middle phalanx to the proximal margin of distal finger joint capsule; Zone II: distal finger joint surface (interior joint capsule); Zone III: from distal side of distal finger joint capsule to free margin of posterior nail fold; Zone IV: form free margin of posterior nail fold to 1/2 nail; Zone V: from the 1/2 nail to the distal end. Grade A: The severed surface is neat without finger contusion; Grade B: The severed surface is not neat with defect and obvious finger contusion, but the blood vessel defect can be covered by shortening phalanx; Grade C: The finger is injured severely by contusion or avulsion, and the soft tissue defect needs tissue grafting or shifting repair.
2. Methods
2.1. Wound debridement, hemostasis and fixation: Perform debridement under sterile condition, use of hydrogen peroxide and other strong stimulant disinfectant should be avoided. The contaminations should be removed carefully from the wound while retaining and protecting viable skin soft tissue. Try to avoid shortening the exposed phalanx and causing new active bleeding while doing debridement. Use Kirschner wire to do intramedullary fixation of the bone fracture, in order to reduce the damage to the blood transportation of the exposed phalanx. Repair the severed tendon and simply suture the viable soft tissue, avoiding skin grafting on the skin and soft tissue defect. If there was active bleeding after wound debridement, loosen the suture in the premise of effective hemostasis in order to guarantee the local blood transportation. Once the bleeding was stopped, remove the stitches as soon as possible.
2.2. Smear MEBO on the wound in the thickness of 1mm, and dress the wound for hemostasis with MEBO oil gauze (every tube of MEBO can be used to prepare 3 pieces of sterile oil gauze). Uncover the dressing after 24h to expose the wound and continue using MEBO once every 4 h~6 h, or keep bandaging method with MEBO dressing changed twice a day. Generally, retrograde and severely contused soft tissues got dark into necrosis in 2 d~7 d, when timely remove necrotic tissues to create a favorable condition for wound regeneration. With the time going, newly growing granulation tissues could be observed on the surface and peripheral area of the exposed bone as well as in the medullary cavity of extremities, covering the exposed phalanx and tendon. With the white epithelial tissue growing around the wound, the wound healed gradually. The longest duration of treatment was up to 3 months.
2.3. Systemic treatment: Administer routinely tetanus antitoxin 1500 IU by intramuscular injection after the reception of negative result of skin test; a dose of 3000 IU was applied for wounds severely contaminated or injured for more than 8h. Then apply penicillin or clindamycin antibiotics by i.m. or i.v. based on the bacteria epidemic report provided by the infectious department of the attending hospital as well as the history of antibiotic use of patients. For fresh wound, apply the above antibiotics in full dose once before debridement, and then continue using for 5 d~7 d and terminate. Then selectively use antibiotics according to the wound condition and bacteria test. For wounds severely contaminated or injured for more than 8 h, continue using antibiotics until no flare or cellulitis of the wound occurred[6].
2.4. Efficacy assessment criteria
Excellent: Wound healed without scar, the injured finger retained the length without ankylosis, the nail and finger print was intact, finger tip was in rich of nerves, whose function restored fast after treatment with two point discrimination between 2 mm~4 mm; Good: Wound healed without obvious scar, the injured finger was shortened but beyond the wound level with part nail and finger print restored; Acceptable: The wound healed on the original injury site with obvious scar, the injured finger was shortened with part nail and finger print restored; Poor: The wound could not heal and required skin grafting or skin flap transfer repairing.
3. Results
All the patients healed with an average healing duration of 5 w, the longest being three months; no case needed skin grafting or skin flap transfer repairing. See table 1~2 below.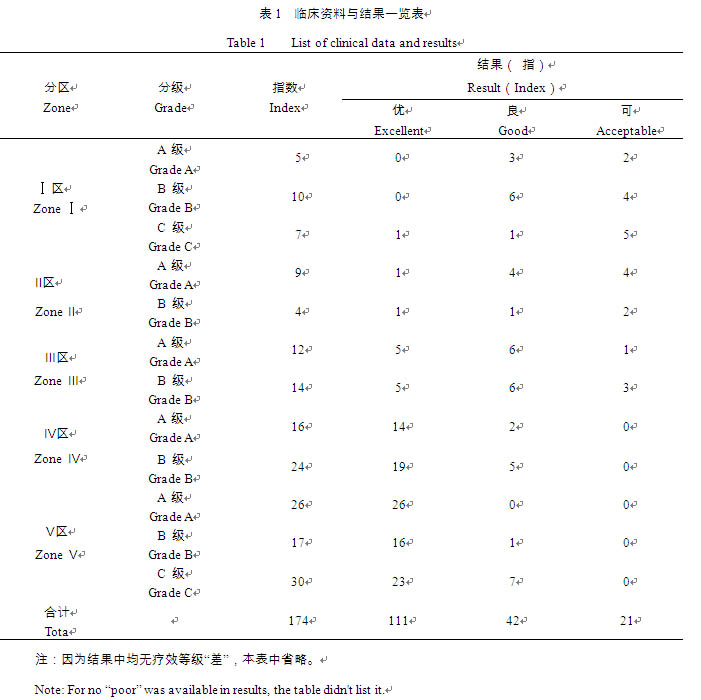
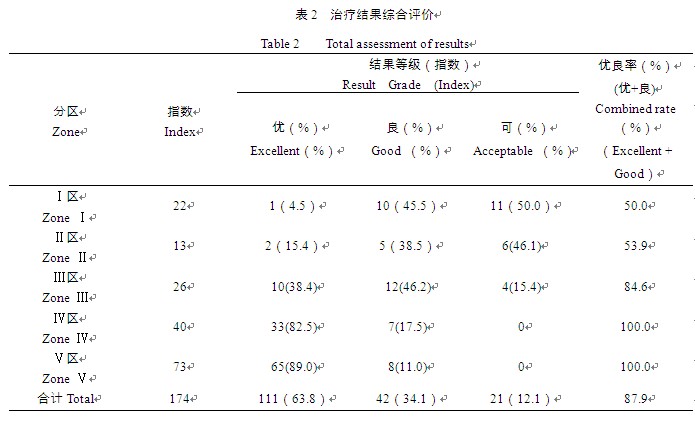
注:1. 因为结果中均无疗效等级“差”,本表中省略;
2. 全组总体愈合优秀率为63.8%,优良合并率达87.9%;
3. 愈合优良率与手指末节损伤程度有关,Ⅰ、Ⅱ、Ⅲ区损伤的优秀愈合率均低于50%,而Ⅳ、Ⅴ区的愈合优良率达100%。
Note: 1. For no “poor” was available in results, the table didn't list it.
2. The total excellent rate of the whole group was 63.8%, and the combined rate 87.9%.
3. The combined rate was related to the degrees of distal finger injuries, the excellent healing rate of injury in Zone I, II, III was all below 50% while the combined rate of Zone IV, V was 100%.4. Discussion
4.1. The irreversible loss of local blood supply of the injured area is the only and definite indication to early stage amputation[7]. Phalangette injury is common in clinic. Due to the hand and forearm are lack of subcutaneous soft tissue, it’s likely to have blood vessel, nerve and tendon injury, open articulation or bone exposure occurring after injury. Stage II surgery is always required by the conventional repairing method, and the current popular methods include various sub-dermal vasoganglion skin flap repairing surgeries[8] aimed at protecting finger outline and functions and adjacent finger or palm pedicled skin flap repairing surgery[8], as well as finger stump debridement and sutura surgery not focusing on protecting finger outline and functions by thorough debridement of necrotic tissues and contused tissues, removing phalanx debris of the stump and burnishing the surface, and then directly perform sutura to close the wound. The former one requires not only equipments, but the mastery of technique and experience on micro-surgery of the surgeon, as well as the condition of the donor site and the grafted site. Some even hold that the fresh wound with good basal blood supply is the only indication of sub-dermal vasoganglion skin flap repairing surgery[9]. The latter one is likely to cause the stump shortened and consequently lead to deformity, outline disfigurement and dysfunction of the finger though it requires less on the surgery procedure, surgeon and the equipment. When adjacent finger or palm pedicled skin flap repairing surgery is applied, the surgical area may be expanded with longer surgical duration and higher expense; moreover, such surgery cannot be applied to wound with severe complex injuries. It’s noted by WEI Jia-guo et al[10] that the phalangette soft tissue contusion injury always damages the blood transportation of the soft tissue, causing ischemia and necrosis, and the blood supply of the phalangette endosteum and periosteum hasn’t been damaged completely at early stage. Early application of MEBT/MEBO should be performed to maximumly protect the blood transportation and prevent necrosis of the phalangette, which benefits bone granulation tissue growth and promotes wound healing. It’s important to preserve the length of the injured finger, and do not hurry to shorten phalangette and harm the hand function simply because of the ischemia and defect of the soft tissue.
4.2. MEBO can eliminate necrotic tissue and promote granulation tissue growth as well as reepithelialization. We obtained favorable clinical results in treating phalangette ischemia and necrosis with MEBO[11]. In addition, we found that application of MEBO immediately after debridement of phalangette injury wound with soft tissue defect and suspected soft tissue ischemia and necrosis may reduce the necrosis area, avoid dryness and necrosis of the exposed phalanx and tendon, as well as accelerate wound healing time. Based on the study result that MEBO could sustain the survival and proliferation of gastric and intestinal tissue explant of embryonic white mouse in vitro[12~13], it is safe to infer that early application of MEBO could survive the ischemic agonal tissue cells, reduce necrotic area and shorten wound healing time.
4.3. MEBO is effective on infection control by inducing the heteromorphosis of E. coli, bacillus proteus, staphylococcus aureus and pseudomonas aeruginosa with depigmentation of pseudomonas aeruginosa and debilitation of productive ability of plasma coagulase of staphylococcus aureus, consequently decreasing the speed of bacteria metabolism and synthesis, interfering their growth and multiplication as well as toxicity action[14]. Excessive debridement, local blood transportation damage and strong disinfectants could impair the regenerative functions of tissue cells, and consequently may increase the local infection rate as well as decrease the wound healing quality. Thus, we suggest that strongly irritative disinfectant or excessive debridement should be avoided in order to protect the blood transportation. During MEBO application, follow the principle of application, i.e. “three no” and “three timely” principle. MEBO is effective on skin soft tissue defect of Zone V of phalangette, and for injuries and defect on the joint and cross-joint site, MEBO could repair the injured wound, but not the joint defect. Therefore, it is recommended phalangette defect at the proximate end of the joint be treated by surgery if it has surgical indication.
4.4. In the past studies, we divided the regenerative repairing process of phalangette defect into four stages: stage of wound necrosis, stage of necrotic tissue liquefaction, stage of granulation proliferation and stage of wound skin regeneration[6]. However, such classification in the repairing process of phalangette soft tissue defect of Zone V is not as distinguishable as in that of Zone I~Zone IV. Sometimes, such classification may overlap with each other.References
[1] Angermann P,Lohmann N. Injuries to the hand and wirst-A study of 50272 injuries.J Hand Surg (Br),l993,18:642~644.
[2] WANG Cheng-qi, WANG Wan-li, ZHANG Jing-liang, et al. Classification of severed finger and selection of its treating methods [J]. Chinese Journal of Microsurgery, 200l, 24: 86~87.
[3] QING Shao-ting, GE Bao-feng, XU Yin-kan. Practical Osteology [M]. the second version. Beijing: People’s Military Medical Press, 1999, 518.
[4] PAN Xi-ze, TIAN Wan-cheng, LU Quan-zhong, et al. Replantation of degloving injury of fingertip [J]. Chinese Journal of Hand Surgery 1998, 14 (4): 207~208.
[5] XIANG Li-yuan, LIU Hui-ren, LI Rui-guo. Replantation and classification of phalangette injury [J]. Journal of Practical Hand Surgery, 2005, 19 (2): 75~76.
[6] LIU Ying-xiang, HE Ren-liang, LI Xin-qi, et al. Skin regenerative reparation in situ on finger skin soft tissue defect [J]. Modern Journal of Integrated Traditional Chinese and Western Medicine, 2007, 16 (19): 2643~2644.
[7] A.H.Crenshaw et al. Campbell’s operative orthopaedics [M]. Shanghai: Shanghai Far East Press, 1991: 153.
[8] SHOU Kui-shui. Selection of hand skin grafting [J]. Chinese Journal of Hand Surgery, 2001, 17 (3): 193~194.
[9] LUO Li-qun, XU Qi-wen, XU Zhi-tai, et al. Reparation of hand and forearm skin soft tissue defect with pedicled sub-dermal vasoganglion skin flap repairing surgeries [J]. Chinese Journal of Reparative and Reconstructive Surgery, 2004, 18 (5): 405.
[10] WEI Jia-guo, SUN Ji-li. MEBO in treating infected bone exposed wound [J]. Journal of Binzhou Medical University, 1998, 10 (4): 515.
[11] LI Gang-sheng. Sixty cases of finger tip necrosis cured by MEBO gauze [J]. The Chinese Journal of Burns Wounds & Surface Ulcers, 2001, 13 (2): 108.
[12] XU Rong-xiang, WANG Yun-ping, FAN Ran, et al. GIC could maintain survival and promote cell growth of organ-type explants of stomach of mouse embryo [J]. The Chinese Journal of Burns Wounds & Surface Ulcers, 2001, 13 (4): 209~214.
[13] XU Rong-xiang, WANG Yun-ping, FAN Ran, et al. GIC could maintain survival and promote cell growth of organ-type explants of intestine of mouse embryo [J]. The Chinese Journal of Burns Wounds & Surface Ulcers, 2001, 13 (4): 215~220.
[14] QU Yun-ying, QIU Shi-cui, WANG Yun-ping, et al. Experimental research on anti-infection effect of MEBO [J]. The Chinese Journal of Burns Wounds & Surface Ulcers, 2000, 12 (3): 44~46.Received Jan. 31, 2011